Ensuring mental health NPs are prepared for rural practice
Department of Health grant assists in addressing provider shortage
November 10, 2020
While nurses make up the largest share of the state of Minnesota’s licensed providers — making them the foundation of the health care system — the majority of them serve in urban areas. As a result, rural communities are experiencing a severe shortage of providers, especially in primary and mental health care. The Minnesota Department of Health (MDH) reports that 80% of the counties in the state are experiencing a mental health professional shortage.
A recent grant award from MDH will enhance the school’s efforts to ensure students in the psychiatric/mental health nurse practitioner program are prepared for rural practice. The initiative will focus on providing more clinical experience to students in rural communities, enhancing the curriculum, enrolling more students who live in rural communities and continuing the Rural Mental Health APRN Conference for education and networking.
“We learned a lot about rural health care as we implemented two Health Resources and Services Administration grants that addressed these issues,” says Professor Merrie Kaas, PhD APRN, PMHCNS-BC, FAAN, who is the psychiatric mental health nurse practitioner program specialty coordinator. “We’ve seen what’s needed and what the challenges are in providing rural mental health care.”
Increasing rural clinical experience
Since 2017, students seeking to become psychiatric/mental health nurse practitioners had the option of completing a two-day short-term experience practicum in a rural community. Beginning this academic year, students in the psychiatric/mental health Doctor of Nursing Practice program are required to complete a 40-hour clinical experience in a rural community. In addition, students will be able to select a rural mental health clinical training residency during their last semester in the program.
“Students who experienced practicums in rural communities were amazed at the resources and the opportunities that are there and the type of patients that they saw,” says Laurissa Stigen, MS, RN, campus system partnerships coordinator. “Over two days they went to five types of facilities that provided some type of mental health care, so I think their eyes were opened to the richness of resources that are available in greater Minnesota.”
A community of providers
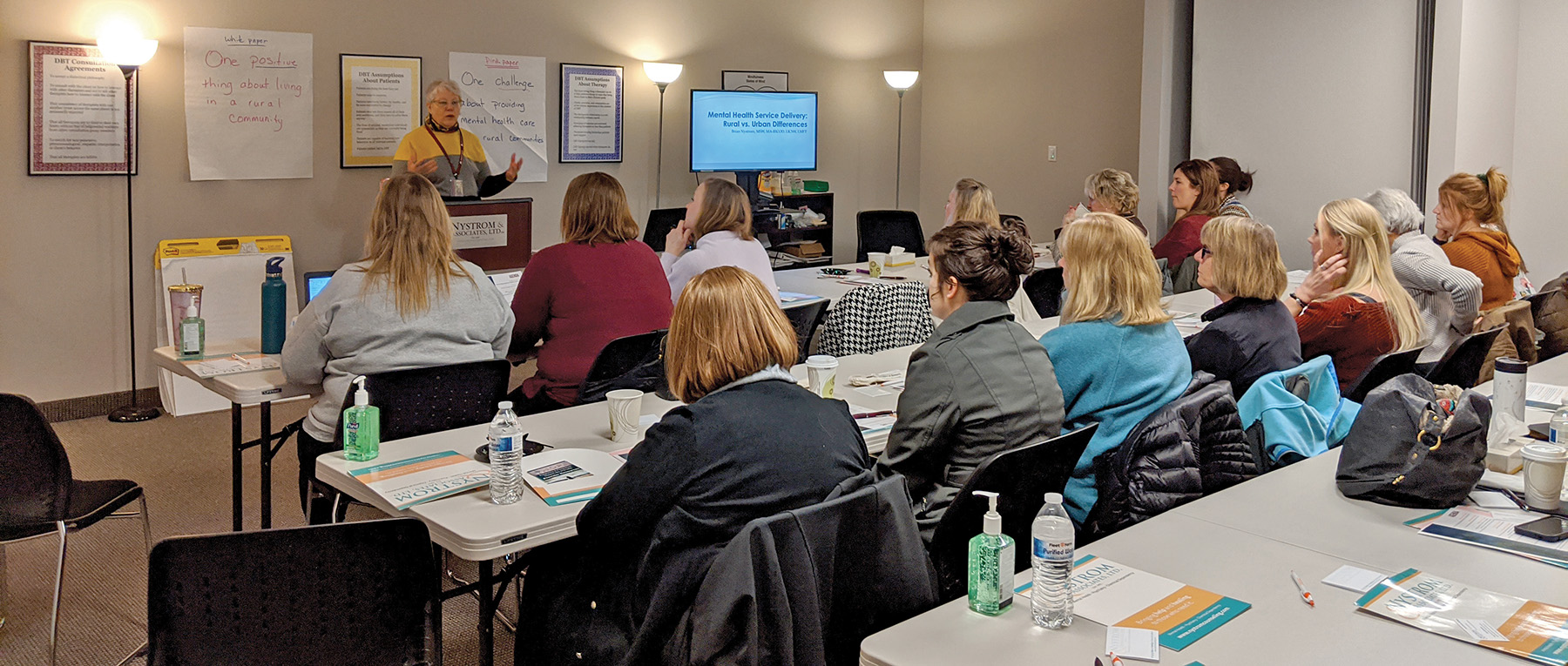
For two years, the school has hosted the Rural Mental Health APRN Conference, which supports providers, students and prospective students to discuss clinical issues in rural areas as well as network with each other for consultation and support. Already a Facebook group was created so that conference attendees can connect throughout the year, and the grant ensures the conference will continue.
“The biggest challenge for many providers in rural Minnesota is isolation. They are working with patients with complex mental health needs, and, for the most part, they’re by themselves,” says Kaas. “We created this conference to build professional networks that can provide resources and connections for our psychiatric/mental health advance practice nursing colleagues in rural communities. Networking is so important in this time of COVID-19 when many providers are working alone from home.”