Going the distance
Researchers are developing a comprehensive pain management program for rural veterans, who have more severe pain than the average person but less access to care
May 13, 2024
Kevin Coss

Chronic pain is a big issue for those who have served in the military.
About 77% of veterans report pain control among their top three priorities in primary care, while two-thirds report that pain significantly limits what they can do and drives them to frequently seek health care.
For those veterans living in rural areas, the picture gets more complicated. Accessing safe and effective care for pain can be difficult. Veterans in rural areas are prescribed more opioid medications than their urban counterparts, and long-term use of these painkillers can lead to addiction or even death through accidental overdose.
“In short, rural veterans are more severely impacted by pain but have fewer options for care,” says Roni Evans, DC, PhD, director of the Earl E. Bakken Center for Spirituality & Healing’s Integrative Health and Wellbeing Research Program (IHWRP). “There is an opportunity to better connect them to non-drug, complementary and integrative health approaches that address pain in a more cohesive way.”
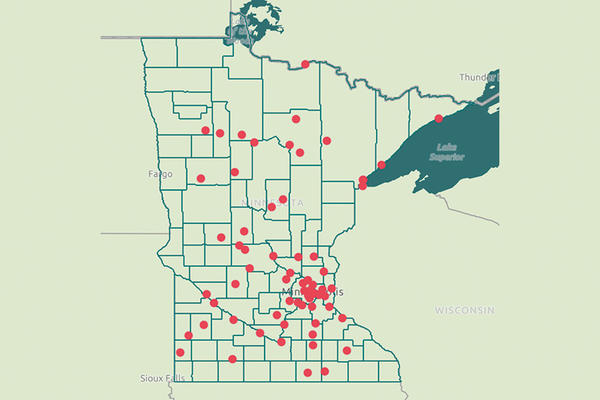
Evans is collaborating with two Veterans Administration (VA)-affiliated researchers to develop and test a program to better deliver care for chronic pain to rural veterans. The team aims to develop a 12-week program called Reaching Rural Veterans: Applying Mind-Body Skills for Pain (RAMP) that includes one-on-one health coaching, video lessons, group discussions and exercises to manage pain in both the mind and the body. The project will be supported by over $4 million in anticipated funding from the National Institute of Nursing Research, part of the National Institutes of Health, as part of the Helping to End Addiction Long-term (HEAL) Initiative.
Instead of relying on medication, the program will draw on evidence-based practices to help veterans understand their pain better, learn cognitive behavioral strategies that change how they view and respond to that pain, and practice exercises that involve movement, mindfulness meditation and other mind-body skills, like progressive muscle relaxation and guided imagery to improve their quality of life.
Addressing barriers that rural patients face
VA patients living in rural areas have unique challenges beyond what their urban-dwelling counterparts experience and are more likely to be affected by pain, says Diana Burgess, PhD, the lead principal investigator on the project, director of the VA Advanced Fellowship Program in Health Services Research at the Minneapolis Veterans Affairs Healthcare System, and professor of medicine at the University of Minnesota.
“Rural VA patients receive over 30% more opioids than urban VA patients, are less likely to receive comprehensive and specialty pain care, in part, due to lack of access, and are less likely to use self-management interventions for pain,” Burgess says. “Our intervention is specifically designed to address barriers that prevent rural-dwelling VA patients from engaging in non-drug, self-management interventions for pain.”
Learning from participants
Over the first phase of the project, the research team will develop community partnerships and pilot test the program.
Katherine Hadlandsmyth, PhD, a co-principal investigator on the study as well as a clinical psychologist and associate professor in the Department of Anesthesia at the University of Iowa Carver College of Medicine, said the input of partners within the VA as well as community groups will help the team design the program to both fulfill national pain care priorities and fit within the day-to-day operations of a busy medical center.
“Working closely with VA partners at both the national leadership level and the local clinician level will ensure that we are building the RAMP intervention in a way that it can subsequently be delivered clinically, should we find it to be efficacious,” says Hadlandsmyth, who is affiliated with the Veterans Rural Health Resource Center at the Iowa City VA. “Meanwhile, including community group representatives offers critical insights into how to engage with varied rural veteran populations and also how to then meet the specific needs of these subsets of veterans.”
During the second phase, the team will conduct a larger study involving 500 patients in the VA health care system to measure how effective the new program is compared to standard care patients have typically been receiving. They will also work with partners to determine how to grow the program within the VA’s national Whole Health System initiative so that it can be expanded to serve rural veterans across the country, including those in underserved and marginalized groups. If the study shows the program to be successful, the VA will be well equipped to implement it on a larger scale.
“We want to ensure that our intervention is serving the needs of a wide range of rural veterans with chronic pain,” Hadlandsmyth says.