Innovative learning experience focuses on transgender patients
Simulations designed to address health disparities
May 6, 2022
Brett Stursa
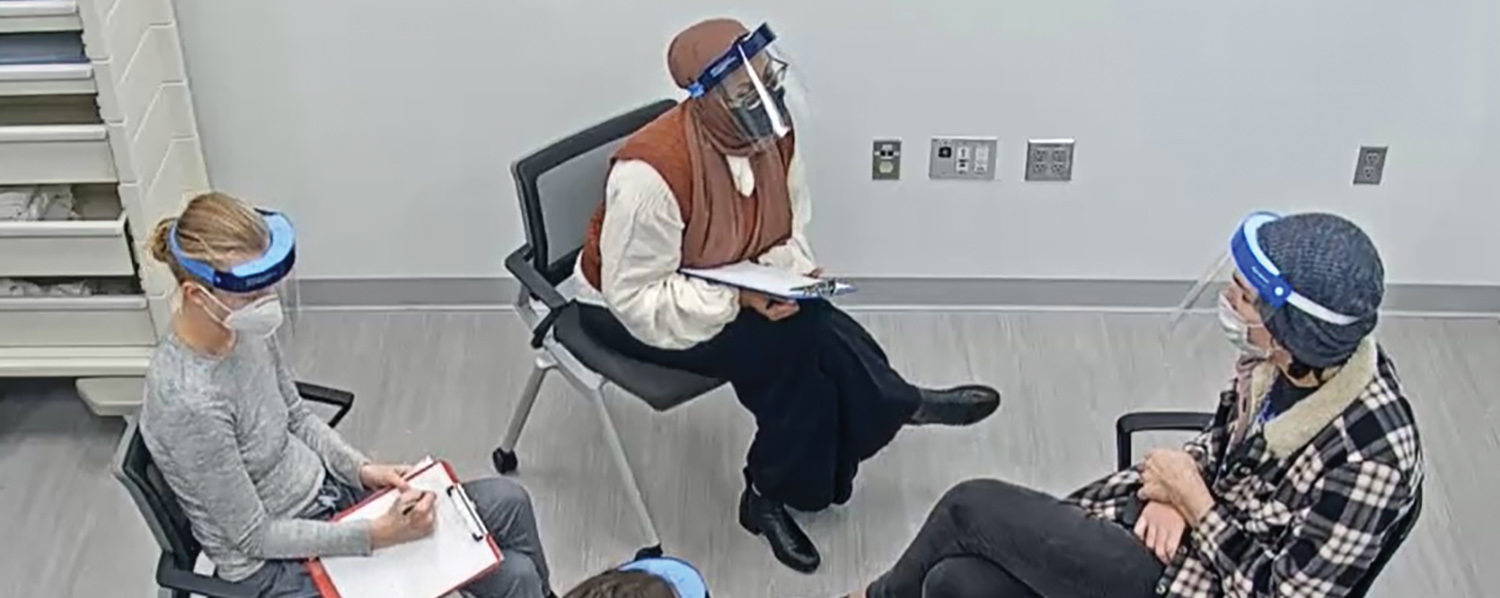
Doctor of Nursing Practice students now have the opportunity to enhance their knowledge, skills and comfort in working with gender diverse populations after the University of Minnesota School of Nursing launched a new interprofessional simulation experience with standardized patients who are transgender and non-binary.

Standardized patients play an important role in the education of nursing students. As actors with scripted histories, they portray patients, allowing students to ask questions and listen in a simulated clinical environment.
A grant from the University’s Institute for Diversity, Equity and Advocacy assisted in the creation a simulation experience for School of Nursing nurse-midwifery and women’s health nurse practitioner students and Medical School obstetrics and gynecology residents. Specifically, students have the opportunity to practice health history techniques.
“Our hope is that students gain a self-awareness on how to interview a patient with cultural humility and be affirming in that process,” says Clinical Assistant Professor Maria Ruud, DNP, APRN, WHNP, who developed the simulation activity with Professor Emeritus Melissa Avery, PhD, APRN, CNM, FACNM, and Assistant Professor Samantha Hoffman, MD.
Addressing health disparities
Transgender and non-binary individuals have significant health disparities and barriers to accessing care, with provider knowledge and training identified as barriers. The simulation experience was developed to increase that knowledge and training.
“These health disparities are not innate but rather are unjust and remediable because many of the negative outcomes are not related to one’s personal identity but are the result of society’s reaction to it,” says Ruud.
Simulations increase students’ comfort, skills
With faculty, M Simulation educators Joe Miller and Anne Woll, Jennifer Demma from Family Tree Clinic and members of transgender and gender diverse populations developed a sexual and reproductive health focused clinical history simulation activity.
Ruud says the partnership with Family Tree Clinic in St. Paul, which is a community clinic known for providing excellent care to gender diverse populations, was critical to the success of the project.
“Working with a provider who was a content expert in health care for transgender and nonbinary people helped to create a simulation experience that was realistic and relevant to best practices,” says Ruud.
The standardized patients, who were transgender or gender diverse, were also involved in creating the scenarios. They were called patient-teachers to acknowledge the broader teaching partnership and the value of their lived experience.
They developed two scenarios — a transfeminine individual, assigned male at birth, who uses she and her pronouns, presenting with urinary symptoms and requesting screening for sexually transmitted infections and a transmasculine individual, assigned female at birth who uses he and him pronouns, presenting with vaginal symptoms and requesting screening for sexually transmitted infections.
“Patient-teachers were key to editing and revising the cases including gender-affirming language as well as planning specific details of the simulation,” says Ruud. Scenarios included non-binary partners and consensually nonmonogamous sexual activity and behavior with multiple partners of various gender identities.
“This identity allowed the learners to practice assessment and understand the distinctly different elements of sexual orientation, sexual behavior and gender identity while emphasizing the importance of not making assumptions about gender or sexuality,” says Ruud.
Students participate in a prebriefing, where they are provided with the presenting case patient’s name and legal name, gender identity and sex assigned at birth, and pronouns as well as presenting symptoms and reason for the clinic visit. Then, after the simulation, they participate in a debriefing.
Ruud recently published the article Health History Skills for Interprofessional Learners in Transgender and Nonbinary Populations in the Journal of Midwifery and Women’s Health, with evaluation of the learning experience.
Evaluation using surveys measured students’ skills and comfort providing care, attitudes about care and overall satisfaction with the simulation learning activity.
Significant differences between pre- and post- simulation were observed for all comfort and skills questions, showing an increase in perceived comfort or skill for all questions. Students reported they appreciated the chance to practice language in a safe environment, which helped ease anxiety and where they didn’t feel judged.
More inclusive, thoughtful language
Ruud says that with each iteration they are learning how to improve the simulations, which are now being utilized with family and adult gerontological nurse practitioner students as well. “I have noticed a difference in the language that students use, even when they’re doing case presentations,” says Ruud. “They’re more inclusive, more thoughtful, more intentional.”
The awareness is key to developing trust and making a patient feel welcome. Without it, Ruud says, there is a concern that patients can get disconnected from the health system and potentially from receiving quality care.
“Health disparities exist in part because transgender and gender diverse people don’t always feel welcomed when they seek care,” says Ruud. “The good news is that we can change that, it is remediable. This is one little step moving in that direction.”